Continued Treatment After Breast Surgery of Lobular Carcinoma
FAQs
Frequently Asked Questions About ILC
These Frequently Asked Questions (FAQs) and their answers about invasive lobular carcinoma (ILC), also known as lobular breast cancer, are for informational and educational purposes. The Lobular Breast Cancer Alliance (LBCA) hopes the FAQs may allow patients and caregivers to have more informed discussions with their health care providers. It is not meant to replace the advice and care patients receive from their health care provider. (Updated and Reviewed: August, 2018)
LBCA can not recommend specific health providers or treatment facilities. There is no objective way to evaluate providers, and every patient and their needs are unique. However second opinions can always be helpful, particularly for cancers like ILC that are less frequently treated at smaller hospitals. A second opinion can be sought for treatment advice, and consults are generally available for radiology and pathology. The National Cancer Institute (NCI) has a network of NCI-Designated Cancer Centers around the country. These Cancer Centers treat larger volumes of patients, see more lobular breast cancer patients, and serve as centers for research and cutting-edge cancer treatments. Find an NCI Designated Cancer Center.
There are currently no unique treatment guidelines for lobular breast cancer, and ILC is treated with the same standard of care as more common ductal carcinomas. LBCA is working to accelerate research to better understand ILC to find targeted therapies and to refine treatments so patients with lobular breast cancer receive care tailored to their disease. Patients with lobular breast cancer benefit from learning as much as they can about their disease so they can be their own advocate and ask informed questions of their health team.
Invasive Lobular Breast Cancer (ILC) is a different cellular type of breast cancer that comprises 10–15% of all breast cancer with up to 40,000 new diagnoses a year in the US. ILC is under researched and can respond differently to commonly applied standard therapies and needs more research to 1) refine current treatments, 2) identify targeted therapies, 3) refine and improve screening methods to detect ILC and its progression, and 4) describe appropriate follow-up care. Patients may not always be informed that they have ILC or its unique challenges. Healthcare providers are not always informed about the differences in the disease and treatment challenges it presents. ILC is frequently not included in breast cancer communications or within breast cancer community resources, is underrepresented at breast cancer conferences and meetings and publications, and is rarely segmented in existing clinical trials and studies with few lobular specific trials. Advocacy for more research requires communications and outreach to raise the profile of this disease with cancer research stakeholders (researchers, clinicians, patients and advocates) to advocate for additional resources for research.
ILC is the second most common histological type of breast cancer comprising 10% to 15% of all breast cancers. Histology refers to the cellular structure of the cancer. In the most common subtype of ILC, classic ILC, cells grow in single file like a string and may not form a lump. Other less common cellular variants of ILC can have different cellular growth patterns. There is growing evidence that some molecular features of ILC are distinct from invasive ductal cancer (IDC), the most common histological subtype of breast cancer.(Cirello et al, Cell 2015).
Invasive Lobular Breast Cancer is the sixth most frequently diagnosed cancer of women in the US.An estimated 44,000 new cases of ILC are diagnosed each year in the US, and approximately 450,000 patients in the US are either currently receiving treatment or have completed treatment for invasive lobular breast cancer. While ILC is often thought of as a "rare" cancer, it impacts more women than cancers of the kidney, brain, pancreas, liver, or ovaries as well as melanomas, leukemias and Non-Hodgkin lymphoma. (Adapted 2018 ACS Surveillance Research, SEER)
Yes. While classic ILC is the most common subtype of lobular breast cancer, there are other histological (cellular) subtypes of ILC that have different cellular structures and variants. Find basic information on ILC subtypes. A more comprehensive explanation Pathology and Genetics of ILC and their Pre-cursers was presented at the ILC mini-symposium at the 2017 San Antonio Breast Cancer Symposium.
There is no current research about how or if different molecular and/or histological subtypes of ILC might respond differently to treatments. Patients who want to know their subtype of ILC should consult their pathology report and their health care provider.
Lobular hyperplasia and LCIS are not considered to be cancer, however both convey a higher risk of developing breast cancer.
Hyperplasia is an overgrowth of cells. "Atypical" hyperplasia means that the cells look distorted when examined. The American Cancer Society offers a comprehensive summary of Hyperplasia and cancer risks.
Lobular Carcinoma in Situ (LCIS) means that cells that look like cancer cells are growing in the lobules (milk glands) of the breast but they are not growing through the wall of the lobules (invasive). LCIS typically does not become invasive, however it does convey a higher risk of developing breast cancer in either breast. The pleomorphic variant of LCIS, however, is a more aggressive variant of LCIS that can often lead to treatment recommendations similar to those for Ductal Carcinoma In Situ (DCIS), or stage zero non-invasive breast cancer. Pleomorphic variants of LCIS have more atypical cells than other types of LCIS.
Invasive Ductal Carcinoma (IDC) is the most common histological (cellular) type of breast cancer and comprises approximately 80% of all breast cancers. IDC has a cell structure that forms a lump in the breast. When it spreads (metastasizes) it tends to spread to the bones, liver, lungs and brain.
Invasive Lobular Carcinoma (ILC) makes up 10 – 15 percent of all breast cancers and is the second most common histological (cellular) subtype of breast cancer. Classic ILC may not form a lump – instead ILC typically causes a thickening of the breast tissue due to cells that spread in single file patterns. ILC is usually (but not always) very strongly Estrogen positive, Progesterone positive and HER2-negative (ER+ PR+ HER2-). ILC is typically considered a slower growing cancer, and has a tendency to recur later than IDC.(Pestalozzi et al, JCO, 2008; Engstrom et al, Histopathology, 2015; Adachi et al, BMC Cancer, 2016; Chen et al, PLoS 2017)
ILC cells frequently experience a loss of the protein E-cadherin. This loss reduces the ability of ILC cells to bond together to form a lump and instead the ILC cells grow in a single-file pattern.(Cirello et al, Cell 2015).
Monthly breast self-exam is recommended self-care for all women, but is not always a reliable way for women to detect their own cancers. Routine self-exams can provide patients an awareness of the feel and shape of their breasts so that to more readily recognize changes and report them.
On self-exam ILC may cause a visual puckering or pulling of the skin or the nipple, unexplained skin hardening, a visual dimpling or dent in the breast, one breast that appears larger or a different shape than the other, or hard areas in the breast that are not easy to move. ILC can, but does not necessarily form a lump. Typically breast cancer is not painful, but sometimes breast pain can be a symptom. ILC often may not be detectable on self-exams at all, particularly when tumors are small. View the Signs of Invasive Lobular Breast Cancer graphic.
ILC often grows in a single-file pattern through the breast tissue without always forming a lump that can more easily be seen on mammography. ILC is more likely to be missed on screening mammograms than ductal breast cancer.(Christgen M, et al. Pathol Res Pract. 2016; Berg WA, Gutierrez L, NessAiver MS, et al., Radiology. 2004; Lopez JK, Bassett LW. Radiographics. 2009, Johnson, K., Sarma, D. & Hwang, E.S. Lobular breast cancer series: imaging.Breast Cancer Res17,94 (2015)
General population breast cancer screening is intended to broadly screen the majority of healthy women who have never been diagnosed with breast cancer. Mammograms are not a perfect screening tool, and ILC can be particularly challenging to detect on a mammogram. The annual mammogram is currently the only recommended general population screening test broadly available for the routine screening of all healthy women.
If a patient or their physician detects any abnormality on self or clinical exam and the mammogram and ultrasound does not show any abnormality, patients may choose to discuss adding an MRI to their evaluation. An MRI is more sensitive than a mammogram or ultrasound in detecting lobular breast cancer. Breast cancer screening recommendations for women who have not had a cancer diagnosis should be based on personal risk factors, such as family history and patient preference. Patients with risk factors may have more extensive screening after discussing the pros and cons with their health care provider.
Tomosynthesis (also known as 3D Mammograms) and/or Screening Ultrasound (SU) increase the detection of all breast cancers. Breast MRI is gaining acceptance as a screening option for breast cancer survivors and women with an elevated lifetime risk of breast cancer due to abnormal biopsies, hereditary mutations, and/or significant family history of breast cancer. (NCCN.org) Patients may want to discuss the pros and cons of these mammogram alternatives with their providers.
Women who have been found to have dense breast tissue on their radiology reports may choose to discuss alternatives to screening and imaging with mammograms with their health providers. Dense breast tissue itself is a risk factor for breast cancer. For women with a history of lobular breast cancer, having dense breast tissue can make finding a recurrence more difficult. Screening Ultrasound and Tomosynthesis (3-D mammography) are both imaging alternatives that increase cancer detection in all women with dense breasts. The American College of Radiology has a fact sheet on dense breasts and imaging (not lobular specific) and issued recommendations for MRI in particular cases for women with dense breast tissue.
Breast MRI can be useful for many women with newly diagnosed ILC before surgery to better define the extent of disease in their breast(Ha, et al. 2018 Radiology).Patients can discuss whether Breast MRI pre-surgery might benefit them with their surgeon.
Imaging and scans available for metastatic ILC are currently the same as imaging for ductal breast cancers, including FDG PET scans, CT scans and bone scans. FDG-PET provides information about glucose metabolism in the body and is a sensitive method for detecting, staging, and monitoring the effects of therapy for many cancers. Computed tomography (CT) uses an external source of radiation to produce 3-D images that demonstrate the size, shape, and composition of organs and abnormalities within the body. Additionally, sentinel lymph node biopsy can indicate whether breast cancer may have spread beyond the breast and metastasized. The American College of Radiology (ACR) issues guidelines for imaging and offers patient oriented educational information about different types of imaging.
The impact of PET/CT on metastatic staging may be lower for ILC patients than for IDC patients.Hogan MP, Ulaner GA. J Nucl Med. 2015 Nov;56 (11):1674-80) Some patients may find it helpful to send their radiology records and scans to an NCI Designated Cancer Center for second opinions. Referrals should clearly specify "lobular breast cancer."
The treatment a patient receives is dependent on many factors, including the size of the tumor, genetic factors, lymph node involvement and the patient's general health and preferences. The standard of care for treatment of hormone receptor positive ILC is typically no different as for hormone receptor positive ductal carcinoma. The National Comprehensive Cancer Network (NCCN) publishes and updates regularly, guidelines and clinical resources that outline standard of care for treatment of all cancers.
More research and clinical trials are neededto understand if refinements in treatment (surgery, endocrine therapy, chemotherapy, imaging, potential future targeted therapies or immunotherapy) might result in better outcomes for ILC patients. Learn more about ILC Research.
Like ductal breast cancer, lobular breast cancer can recur anytime after initial treatment ends. However, research shows that ILC can often recur years after initial diagnosis. Given the potential for later recurrence, patients may consider discussing with their health provider whether this potential for later recurrence should be considered when weighing the pros and cons of extending the number of years they receive adjuvant endocrine therapy (such as Tamoxifen or an aromatase inhibitor).(Pestalozzi et al, JCO, 2008; Engstrom et al, Histopathology, 2015; Adachi et al, BMC Cancer, 2016; Chen et al, PLoS 2017)
When any breast cancer spreads to distant tissue and organs outside of the breast (or metastasizes) it is considered metastatic breast cancer. All metastatic breast cancer is treatable, but considered incurable.
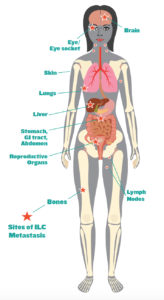 The bones are a common metastatic site for all breast cancers, including ILC. ILC can spread to unusual sites, including the GI tract (stomach, intestines), pleura (lining of the lungs), peritoneum (lining of the abdomen), the ovaries and more rarely orbital metastasis (the soft tissues of the eye). ILC can also spread to other organs common for IDC breast cancer metastasis such as the lung, liver and brain. (Arpino et al, Breast Cancer Research, 2004; Mathew A et al GebFra 2017; Raap et al Cancer Med. 2015, He et al AJR 2014) Visit our For Patients page for more information.
The bones are a common metastatic site for all breast cancers, including ILC. ILC can spread to unusual sites, including the GI tract (stomach, intestines), pleura (lining of the lungs), peritoneum (lining of the abdomen), the ovaries and more rarely orbital metastasis (the soft tissues of the eye). ILC can also spread to other organs common for IDC breast cancer metastasis such as the lung, liver and brain. (Arpino et al, Breast Cancer Research, 2004; Mathew A et al GebFra 2017; Raap et al Cancer Med. 2015, He et al AJR 2014) Visit our For Patients page for more information.
Bone pain, abdominal pain, abdominal distention and/or bloating, unexplained shortness of breath, unusual pelvic bleeding and unexplained weight loss would be some concerning symptoms to report to a doctor.
There is no unique standard of care for the treatment of metastatic ILC. It is treated in the same manner as other types of metastatic breast cancer. For example, Hormone Receptor Positive (ER+ PR+) ILC metastatic breast cancer receives the same treatment as (ER+ PR+) IDC metastatic breast cancer. The National Comprehensive Cancer Network (NCCN) publishes and regularly updates, guidelines and clinical resources that outline standard of care for treatment of all cancers.
More research and clinical trials are neededto understand if refinements in treatment (surgery, endocrine therapy, chemotherapy, imaging, potential future targeted therapies or immunotherapy) might result in better outcomes for ILC patients. Two clinical trials on metastatic ILC are underway in Europe. Learn more about ILC Research.
A germline (hereditary) mutation in the CDH-1 gene can cause a hereditary syndrome of diffuse gastric cancer (HDCG) and lobular breast cancer. Most patients with ILC will not test positive for this rare mutation. The National Comprehensive Care Network (NCCN) has specific criteria to determine if testing is indicated. More information onrisk of developing lobular for inherited CDH1 mutation carriers.No Stomach for Cancer and an advocate run websiteHeriditaryDiffuseGastricCancer.org might be helpful resources for CDH-1 genetic mutation carriers to learn more.
Somatic testing of metastatic tumors to look for tumor-specific mutations has gained popularity as an attempt to tailor treatment to individual patients. It has limited applicability thus far in breast cancer generally. Somatic testing should be discussed with a health care provider.
ILC is typically a strongly estrogen-sensitive disease. Patients with ILC should consult with their oncologist before taking prescription or homeopathic medications or supplements that contain or mimic the hormone estrogen, including hormonal replacement therapies to relieve menopausal symptoms, supplements or other products that contain or mimic estrogen. General healthy lifestyle recommendations also apply to patients with ILC, including a healthy diet, avoidance of weight gain (estrogen is made in fat after menopause), exercise, and stress reduction. Alcohol moderation or avoidance is advisable, as alcohol has been shown to increase estrogen levels in some studies.
Yes. Find information about ILC trials and studies and links to clinical trial search tools and information to determine whether a trial is a good option.
Lobular breast cancer is an understudied, unique subtype of breast cancer. Clinical trials are needed to better understand this disease and refine treatments. Pre-clinical research is critical to better understand the disease biology and behavior and potentially to identify targeted therapies. Patients can help advance research by participating in studies as appropriate and working with their doctors. Patients can also become a research advocate to advance research, raise awareness and educate others about ILC.
Lobularbreastcancer.org has a variety of information about lobular breast cancer. LBCA has also compiled apublications library of research and studies on lobular breast cancer and resource list of educational and support resources for patients.
Thes FAQs are for informational and educational purposes only. Information found on this page or links should never replace professional medical advice.
Source: https://lobularbreastcancer.org/faq/